Cleaning Your CPAP Machine Proper CPAP cleaning is essential to lowering your risk of respiratory infections when using your CPAP. Cleaning and maintenance are essential for keeping your equipment running at top performance and maintaining its durability. So, let’s examine why, when, and how you should clean your CPAP!
Why Is It Necessary to Clean Your CPAP Machine?
Your cpap machine works hard to deliver a steady stream of air pressure into your airway. The air is frequently humidified, which provides an ideal environment for mould and germs to develop and multiply. Over time, dust and allergens can contaminate your CPAP supplies. These microorganisms can be inhaled when you breathe, making you ill or triggering allergy symptoms. Oils and dead skin cells from your face and hands can accumulate on your mask, causing discomfort and a poor seal. Cleaning your CPAP equipment regularly will also help it last longer.
Related: The main causes of sleep apnea
Cleaning your CPAP equipment regularly may help them live longer and may cure typical CPAP problems like noise and skin irritation.
How Do I Clean My CPAP Machine?
What if you’ve recently recovered from a cold and want to ensure that no unpleasant bacteria remain on your CPAP machine? The good news is that washing your machine, mask, and parts with warm, soapy water should be sufficient to clean and disinfect them. Vinegar may be used as a natural disinfectant after thoroughly washing with soap. If you are particularly concerned about bacterial or viral infection, you should use a specialist CPAP cleaning solution that includes germicide, but don’t use bleach or any other home chemical cleansers. These may leave dangerous residues that irritate the skin or emit poisonous odours.

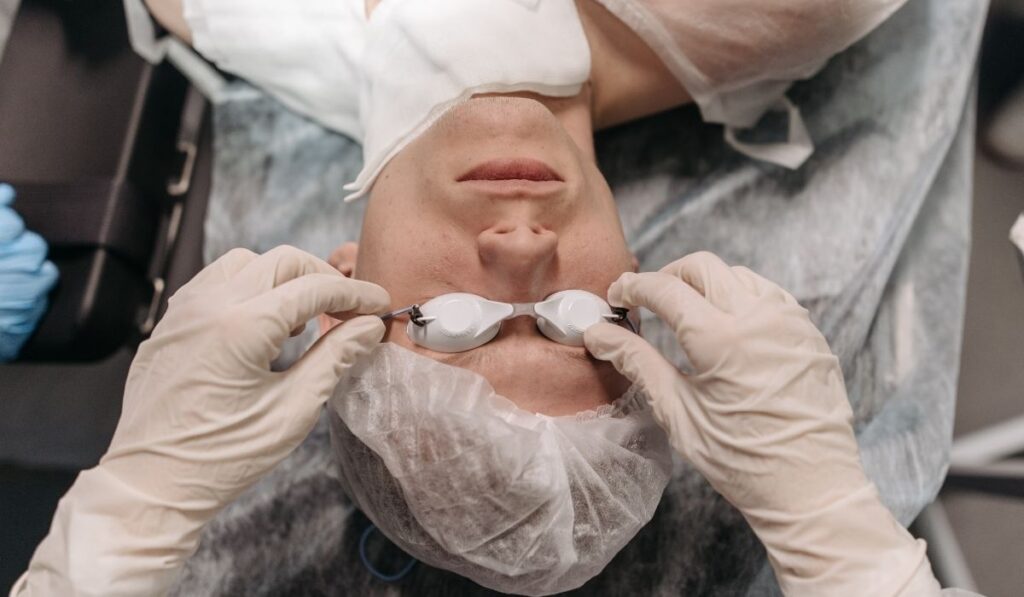
You should also think about using a CPAP sanitizer. These devices use ozone or UV radiation to safely and easily eliminate over 99 percent of viruses, germs, mold, and fungus. However, a sanitizer should be used in addition to regular cleaning. They will not, for example, eliminate any accumulation of oils, skin cells, or mineral deposits and should not be used in place of regular washing.
Cleaning a CPAP Machine
According to the manufacturer’s instructions, your CPAP machine and supplies should be cleaned regularly, or at least once a week. However, if you are unwell, a daily cleaning regimen is essential until you recover.
To clean your CPAP, follow these steps:
- Clean your CPAP supplies first thing in the morning to let them air dry.
- Unplug your gadget and disassemble its components, including the water chamber. Then, using a clean, dry cloth, wipe the outside to eliminate any dust or dirt.
- Use a gentle soap like Dawn or Ivory.
- Use warm soapy water to clean your CPAP mask, tubing, and water chamber.
- Use clean water to rinse your CPAP hose and other accessories.
- If you like, you may use vinegar to disinfect the accessories after they’ve been washed. Soak them in a solution of 1-part vinegar to 3 parts water for around 30 minutes. Then, rinse well with clean water.
- Allow all items to dry naturally.
Important Things to Note While Cleaning Your CPAP Machine:
- Only use distilled water to reduce mineral and bacteria buildup in your CPAP humidifier.
- Consult the manufacturer’s instructions for cleaning your CPAP filters. You can use warm water to rinse some. And you must replace other throwaway parts.
- Never use a dishwasher to clean your mask or tubing. Dishwasher-safe water chambers are possible. To find out, see the manufacturer’s instructions for your CPAP.
- Do not put your helmet or straps in the dryer.
- To avoid discoloration, avoid drying CPAP equipment in direct sunlight.
- Keep in mind that you must still update CPAP supplies regularly. If you are unclear about your replacement schedule, contact your provider.

How to Quicken the Cleaning Process
Don’t worry if you don’t have time to clean your CPAP items weekly. CPAP cleaning alternatives and accessories are available to decrease cleaning time and effort.
If your cleaning practises fall short of the manufacturer’s guidelines, a sanitizer might alleviate your concerns about bacteria or mould buildup. There are several alternatives for the best CPAP sanitizer, but the top customer favourites are the SoClean, the Motif Clean-Z, and the Lumin.
Ozone-based cleaners may violate the warranty on ResMed CPAP equipment. Always consult the manufacturer’s instructions before using a CPAP sanitizer.
Using CPAP wipes might help to prevent buildup on your mask and machine. These should not be used in place of your regular weekly cleaning, but they can assist in preventing dirt buildup and make cleaning easier.
CPAP Spray: A CPAP spray may be used to remove dust and bacteria from your mask and refresh it.
Using the Lumin CPAP Sanitizer
With the strength of specialised UV light technology within the Lumin CPAP cleaner, you can kill viruses, mould, fungus, and more in as little as five minutes. Put your CPAP equipment inside the Lumin, and it’ll be germ-free in no time.
It is the most efficient method for removing 99 percent of germs from your CPAP supplies. You may also use it to sterilise everything that fits within, such as toothbrushes, children’s toys, hearing aids, and other items, without harsh chemicals or water. Look into CPAP cleaner reviews to see which one will best meet your needs.
Do you require new CPAP accessories?
Air Liquid Healthcare covers all of your sleep apnea needs through insurance, from CPAP machines and masks to tubing and filters. Access our user-friendly patient site, and benefit from world-class resources such as our AI mask-fitting technology.