Cataract surgery is conducted when diabetics’ blood glucose levels are well maintained. If blood glucose levels aren’t controlled properly, the surgery is postponed.
Due to postoperative problems such as delayed wound healing and higher infections, diabetic individuals with poor glycemic control are unable to undergo cataract surgery.
Traditionally, hospitalization has been recommended to help with blood glucose control. However, because to small-incision phacoemulsification cataract surgery, which many diabetics receive, same-day surgery has become commonplace. Surgery with a small incision induces less irritation than traditional extracapsular cataract extraction7, and postoperative retinopathy or maculopathy development is uncommon.
However, there are no definite cutoff points for HbA1c levels at which cataract surgery is considered safe and postoperative problems such as retinopathy and maculopathy progression may be avoided. Click here to stay out of complications with these cataract surgery recovery tips.
Preoperative and postoperative blood glucose management for diabetic patients having small-incision phacoemulsification cataract surgery is discussed in this article.
Hypoglycemic patients: surgical problems
Prior to cataract surgery, Japan’s treatment strategy was to maintain blood glucose under control and HbA1c below 10%. Until HbA1c hits this level, surgery is postponed. So, how do you feel about same-day surgery? If blood glucose is properly maintained, hyperglycemia, delayed wound healing, and infection are less common. 3-6, as well as a decrease in postoperative ocular inflammation13 and the occurrence/progression of retinopathy.
Postoperative hyperglycemia is caused by stress and surgery.
According to one research, minor surgery performed under local anesthesia had no influence on blood glucose or cortisol levels. Blood glucose levels will stay steady throughout and after phacoemulsification cataract surgery.
Due to fasting before cataract surgery, these alterations seemed to be connected to differences in oral hypoglycemic and insulin regimens. We don’t believe that fasting before surgery is necessary, and we’ve had no problems operating on diabetic patients who haven’t changed their diet or medications.
Following a subconjunctival steroid injection at the completion of cataract surgery, blood glucose levels tend to be somewhat increased on the day of surgery. After successful cataract surgery, the severity of aqueous flare is comparable in patients with and without subconjunctival steroids. It is not essential to inject steroid into the conjunctiva.
Collagen production is decreased in hyperglycemic rats during wound healing, while insulin normalizes collagen production.
Our 3.5-mm incision heals rapidly and produces less collagen. However, postoperative infection is a major risk.
Diabetic patients had a higher rate of postoperative infections (10.7 percent vs. 1.8 percent), and there was a link between acute postoperative infection and blood glucose levels.
The most dangerous eye infection is postoperative endophthalmitis. Diabetes and postoperative endophthalmitis are not well understood. Although diabetes is not a known risk factor for postoperative infection, diabetics had a higher rate of postoperative endophthalmitis. Surgical endophthalmitis affects diabetics at a rate of roughly 24 percent. There is no documented relationship between blood glucose control and surgical endophthalmitis.
Ocular surgical complications
Following cataract surgery, inflammation is a significant problem. Diabetics have more severe symptoms than those who do not have diabetes. 18 The inflammation after small-incision phacoemulsification cataract surgery in diabetics with mild retinopathy is comparable in diabetics and non-diabetics.
Although postoperative retinopathy and maculopathy are frequent complications, no research has looked at the influence of preoperative blood glucose control. Despite the fact that the development of maculopathy has a considerable influence on postoperative visual results, this topic has received little study and there are no conclusive solutions.
We’ve seen folks who underwent surgery and had a poor postoperative visual prognosis due to poor glucose management.
We looked over these patients’ cases and discovered the following.
The participants in our study were divided into three groups: those who improved their glycemic control quickly before surgery and maintained it afterward (group 1), those who had poor control before and after surgery (group 2), and those who had good control before and after cataract surgery (group 3). (group 3). (3rd group)
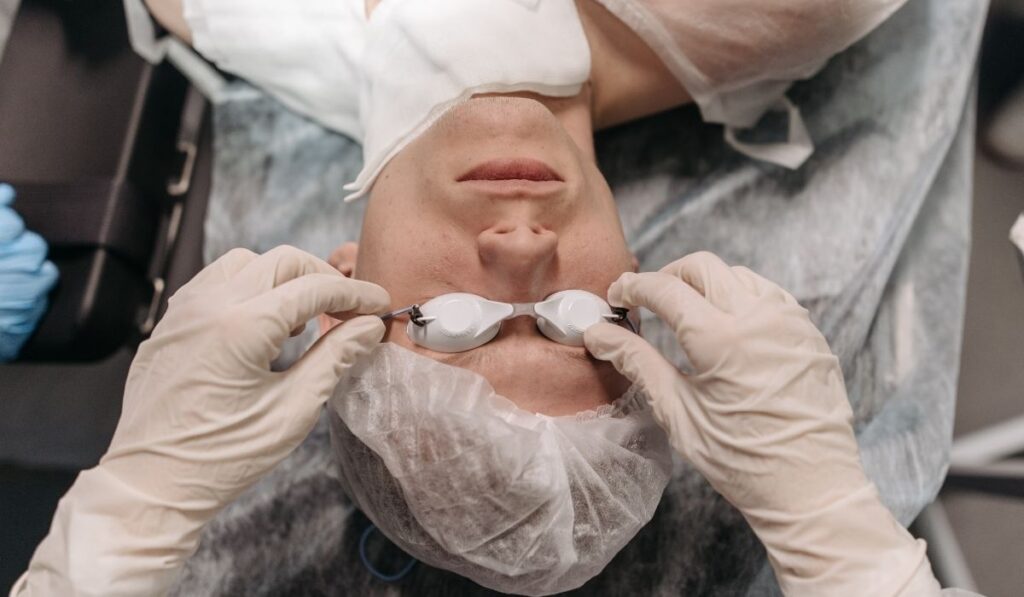
We performed small-incision phacoemulsification cataract surgery in one eye and then tracked the development of retinopathy and maculopathy in the other eye for a year. The small-incision phacoemulsification cataract surgery with acrylic IOLs had no problems. Ophthalmoscopy and fluorescence fundus angiography data were utilized to measure changes in retinopathy and maculopathy using the ETDRS scale.
The development of retinopathy after surgery did not vary between the groups (P=.27). Before cataract surgery, the group with fast glycemic control had considerably higher postoperative maculopathy advancement than the other two groups (P=.02).
Before surgery, the progression of retinopathy and maculopathy in group 1 diabetic retinopathy patients with moderate-to-severe nonproliferative retinopathy (P=.002 and P=.008). Patients with poor glycemic control exhibited no difference in retinopathy advancement at 1 year postoperative compared to the other groups after quick glucose correction, although maculopathy development was more prevalent.
These data suggest that rapidly reducing blood glucose levels before surgery does not help avoid postoperative complications and may significantly aggravate retinopathy and maculopathy in people with mild to severe nonproliferative diabetic retinopathy.

Rapid-correction aspects
Why is it that quick glucose correction causes problems? To prevent diabetic retinopathy from progressing, long-term blood glucose management is essential. After fast and severe blood glucose management, some patients’ retinopathy deteriorated. Japan is dealing with comparable difficulties. This is referred to as early worsening, and it happens a lot once you start insulin treatment. It causes transient visual loss and may lead to proliferative retinopathy, which is permanent.
If stringent blood glucose management, which most physicians and ophthalmologists feel is excellent, promotes retinopathy development, this is a major problem. In individuals who have not been treated for a long period or who have poor glycemic control, retinopathy development is typical following quick blood glucose correction. Blood glucose reduction rate, HbA1c before therapy, retinopathy severity, and diabetes duration are all factors to consider. The specifics of the mechanism remain unclear.
Patients who had no previous retinopathy or had basic retinal seldom progressed after receiving rigorous insulin treatment, whereas those with severe retinopathy did.
Furthermore, the degree of retinopathy before to quick blood glucose control correction seems to be a significant determinant in the ultimate prognosis after rapid correction. Reduced oxygen-release capability of red cells caused by reduced blood glucose levels, as well as generation of hypoxia-inducible factor-1 alpha following insulin treatment, seem to be associated to the advancement of retinopathy after rapid blood glucose management. This is supported by recent study.
The term “rapid correction” has numerous connotations. A 3.0 percent drop in HbA1c within 6 months, according to Kumamoto et al, should be avoided. Retinal edema, hemorrhage, and soft exudates in the central fundus are prevalent in patients with HbA1c values below 3.0% for 3 months. The risk of retinopathy increases if HbA1c lowers from 0.5 to 1.0 percent in a month. Maintaining a monthly HbA1c reduction of 0.5 percent may be difficult.
Conclusion
Nobody knows what the optimum diabetic cataract surgery preoperative glycemic management approach is. In patients with moderate-to-severe nonproliferative diabetic retinopathy, preoperative glycemic management should be avoided because it increases the risk of postoperative retinopathy and maculopathy development. Individuals with moderate-to-severe nonproliferative diabetic retinopathy may also undergo surgery without requiring glucose control. Patients with nonproliferative diabetic retinopathy or maculopathy that is mild to severe may need surgery to enhance their eyesight.
